Not sure where to start with the Keto Diet?
Complete this free 1 minute consultation form to find the perfect plan for you.
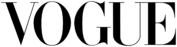
CONSULTATION FORM > Convenient ready meals delivered to you
Convenient ready meals delivered to you
 100% Natural, 100% Keto
100% Natural, 100% Keto
 No Tracking, No Meal Prep, No Food Waste
No Tracking, No Meal Prep, No Food Waste
Sign up to our newsletter
Receive exclusive offers, discounts and news about new product launches straight to your inbox.
Featured in